FIRST PERSON | LEDA MEREDITH
When I landed at SFO in mid-April of last year, the first change to hit me was that my dad, Kelly Johnson, couldn’t pick me up at the airport. He wasn’t able to drive anymore. The reason for the visit to my hometown was that he had gone into hospice care. I’d canceled everything on my schedule and come to be with him. We didn’t know how much time we would have together.
Seeing the elevator chairs that had been added to the two flights of stairs in his Victorian building was a jolt, as were the tubes in his nose; he was on full time oxygen at that point.
But every detail of the home was familiar — from the books on the shelves to the ceramic owl container that he used to hide an Easter egg in when I was a kid.
Neither of us knew then that he would choose to die in less than a month, embracing California’s End of Life Option with gratitude, courage and relief. As he sat hunched over his desk trying to summon up the appetite to finish a piece of toast, we couldn’t have imagined the next few weeks would become a nonstop musical and gustatory celebration with friends.
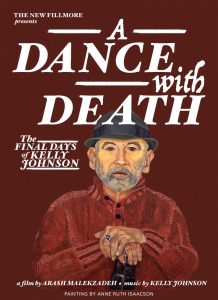
A Dance With Death screens May 7
As part of a year-long series on death and dying, the Main Library will screen the documentary A Dance With Death: The Final Days of Kelly Johnson on May 7, the first anniversary of his death. The screening is part of a program from 5:30 to 7:30 p.m. called “How to Die in California.”
Doctors and hospice workers say it’s not uncommon for terminally ill people to experience bursts of robust health just before they die. In my dad’s case, increased dosages of steroids and painkillers may have contributed.
But I believe it was also the love he was surrounded by — and the peace that he’d made with his past; so many stories I’d never heard before came out near the end. Also, for the first time in years, he had the power of choice and was in charge of his life. His physical health had deteriorated beyond control, but he got to choose when and how to make his exit. And he did so with his usual flair.
One of the ways my dad made peace with his impending death was to organize his life into eras that he could look back on with pleasure and pride. On his website, you’ll find them: the Chicago vaudeville circuit, the San Francisco Dance Theater days, the Berkeley Symphony days and his classical piano concert days.
Organizing these eras, and the combined self-image that he created, became extremely important to him. It was how he embraced his memories and himself when the end was an actual event on his calendar.
It took me a while to understand this and I made some blunders. For example, there was the matter of the bread seeds. Years ago my dad baked a lot and, for several years, anytime he went to a party he would bring what he called The Seeded Loaf. This was a delicious, oblong loaf of bread with an array of seeds sprinkled over the crust: poppy, caraway, sesame, anise. He kept the jars of seeds on the lowest of several spice shelves in his kitchen.
My dad had asked me not to remove or give away any of his things while he was still alive. “I know it’s going to be more of a pain for you to deal with afterward, but I don’t want my home disappearing around me while I’m still in it,” he said.
I imagined how grim things such as the outlines of absent paintings on the walls could be and thought I understood completely. But I didn’t realize that the bread seeds were in the same category.
One day I opened a jar and noticed that the sesame seeds had gone rancid. He hadn’t baked The Seeded Loaf in years, so I didn’t see any harm in throwing them out. Big mistake. He let me know that the jars of seeds were a reminder of the years when he was the guy who would show up at the party with The Seeded Loaf tucked under his arm. After that, I was careful not to get rid of anything in the apartment.
The transformation my dad accomplished during his final days included going from someone who had been wearing the same jeans and hoodie for months to a semblance of the dapper, well-dressed man he’d once been. In the documentary film about his final days, A Dance With Death, there is a scene in which he has several colorful shirts hanging on the Japanese tansu in his bedroom. In the film, he says he remembers where he wore each of them, and how he felt when he was wearing them.
For his death, he chose a button-down shirt with musical notes on it and white cotton pants. This was the outfit he wanted to wear on his trip to Peet’s on that final morning. When he chose it, I pointed out that San Francisco weather is fickle, and he might be cold in such light clothing. He said: “I don’t care. I’m going to go out looking good.”
The day before my dad’s death, his health tanked. Gone was the robustness of the past two weeks. Doubled was the quantity of painkillers he required. He told me he wasn’t sure he was going to make it to his planned demise the following day. He also told me: “I’m glad I feel awful today. I had started to forget why I wanted to die.”
On the morning of May 7, 2018, Kelly Johnson went out the front door at 2217 Fillmore Street for the last time. It was a glorious sunny morning, with dozens of friends waiting, and jazz diva Kim Nalley sang.
There is one detail that comes back to me again and again. As my husband wheeled my dad’s chair down the street to meet his friends waiting at Peet’s, I walked backward in front of him tossing pink and orange feathers. “We used to put those on our Christmas trees!” he exclaimed with a surprised and delighted smile. He had always been fond of that quirky family tradition.
Later that morning, as we got ready to take him back home for his final hours, one of his friends told me she had spotted a bird flying off with some of those colorful feathers. I like to think the nests in the trees around Fillmore Street were more colorful than usual last spring.
He would have loved that.
An example to others
My dad wanted to be an example to others suffering from terminal disease, as well as their caregivers. He wanted them to know that they could spend those last days celebrating love and memories, rather than slipping inexorably into ever-increasing physical pain and psychological despair.
That said, California’s end of life option is not for everyone. For starters, to qualify for the program, two doctors have to affirm that the person’s illness is incurable. My dad’s long-time primary doctor refused, and he had to find another.
The person must also be of sound mind and able to have clear conversations with hospice workers and doctors. In my dad’s case, these conversations took place over the three weeks before the date he had chosen for his death. They included questions such as: “Are you still sure you want to do this?” and instructions about what the process would be on that last day.
The physical process for dying under the law is that the person first takes an anti-nausea medication, then the contents of 90 capsules of Seconal emptied into a glass and mixed with juice or other liquid. The person must be able to lift the glass on his or her own. If the person is too physically weak, a caregiver may hold the glass, though the person must drink the mixture through a straw; no one else can empty it into his or her mouth. The person choosing to die must still be clearly acting of free will. In addition, an official witness must be present. For my dad, it was one of the hospice nurses.
The end was painless: My dad drifted off to sleep almost immediately and within minutes was dead, although we had been warned by hospice workers that in some cases it takes longer.
From my experience, the most important thing I can advise caregivers is that in the weeks before the death, it really does take a village. I was my dad’s primary caregiver during those final days, but I had help from friends and neighbors, my husband and the hospice team. Even with all of that, during the last week I hired a night nurse because I had been keeping an ear out in case my dad needed something in the middle of the night. It is stressful to know that you are about to lose a loved one who is so very important to you. In my case, it helped to ask my dad’s friends to spend time with him while I went to a yoga class every day.
Be aware that some of the well-meaning people around you may have strong objections to the end of life option, for religious or other reasons. They are likely to hit you with their objections rather than confronting the dying person with them. Also, you and others may have the urge to take care of the person in ways that are no longer meaningful. For example, if a person with only a few days to live wants to eat something you consider unhealthy, allow it.
Most important of all: listen. Some of the stories my dad wanted to share at the end were shockingly personal. Others I had already heard a thousand times. It didn’t matter. What mattered was that people who loved him were there to listen to the story of his life as he remembered it.
Finally, know that the group Compassion and Choices is a useful resource for people considering the end of life option, as well as for their caregivers.
— Leda Meredith
EARLIER: “The final days of Kelly Johnson“
Filed under: First Person, Locals